We know how antibodies perform in our body to restrict the foreign invasions, so that we can protect ourselves from various illnesses caused by viruses and bacteria.
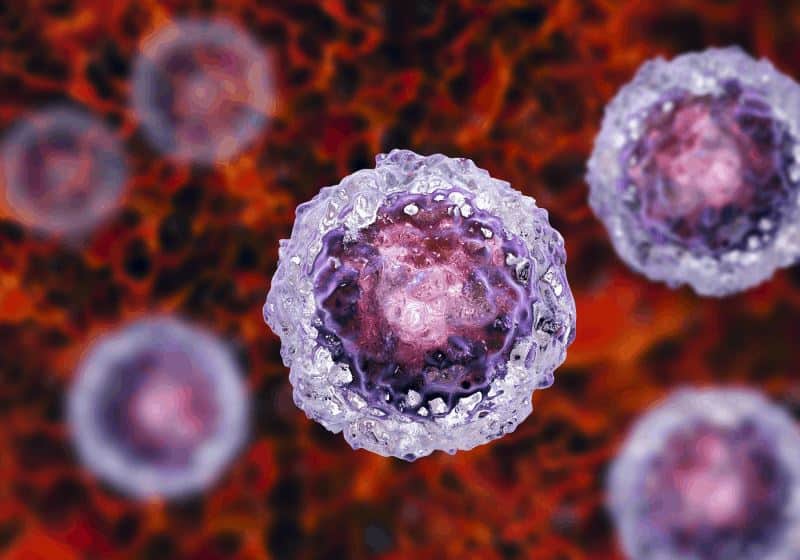
Other than these usual physiological activities, they are found to have lent their hands in the development of Induced Pluripotent Stem Cells by using external parameters. This, we can take as a major breakthrough in the field of medical science, which could be effective in producing different drugs, and medicinal therapies to combat a range of diseases.
In a recent research by the scientists at The Scripps Research Institute (TSRI), it has been proved that antibodies could be a useful component to a new approach as “reprogramming” ordinary adult cells into stem cells or induced pluripotent cells. And to do the “reprogramming” techniques into the DNA’s of the adult cells, no invasive procedures are needed to be followed as is with the “reprogramming of stem cells in the human body”.
We already have an insight into how induced pluripotent cells act to differentiate into any cell types and proliferate in the body. With potentials like self-renewal, iPSCs are ideal to be used as a model to identify the etiology of diseases, find new drugs or therapy using stem cells of patients. However, the same functions can be executed by the human antibodies too. This is what scientists at the Scripps Research Institute (TSRI) have focused on this new development. The finding of the study has been made available online in the Nature Biotechnology.
Why Antibodies are Better Than iPSCs?
The process of developing iPSCs involves a manipulation of the genome in the DNA of fibroblasts, found in the skin or connective tissues. These cells could easily be converted into stem cells or iPSCs by adding four transcription gene factors of the DNA of these cells. However, the antibodies as found by the scientists do not follow the same path once introduced to the mature cells, and replace three key transcription gene factors to bind to the proteins of the cells.
Using four transcription genes,s including Oct4, Sox2, Klf4 and c-Myc into the nucleus of the mature or adult cells derived from the patients’ own cells, iPSCs are developed for a variety of medical purposes, say organ regeneration or cell therapies. There have been a few evidences of risks of producing iPSCs cells, hence we fail to experience much practical use of these cells in the medical field.
The development of iPSCs cells depend on the OSKM theory, meaning using these four protein factors and encoding them, they reprogram cells into induced pluripotent cells.
However, the insertion of those proteins into the genes can invite the attack of viruses, or overproduction of nuclear manipulation techniques may cause cancer to the DNA cells. On the other hand, the production of iPSCs through nuclear reprogramming fosters the collections of different variable properties.
While antibodies do not use any extra DNA as iPSCs to reprogram mature cells into stem cells or iPSCs, it takes into account only three key transcription gene factors excluding the fourth transcription gene factor Klf4.
Hence, iPSCs derived from antibodies could have fewer mutations, and better properties to be used as an effective model in the lab.
The Process Of The Study
The research was carried out on a collection of 100 million human antibodies to examine if any of the antibody could develop iPSCs by replacing OSKM transcription factors. The process was examined on the fibroblasts of mice, and cultured in the lab using first two factors of OSKM such as Oct4 and Klf4. Later on, the entire library of antibodies was placed in the culture tray to find a replacement of functions of other two gene factors such as Sox2 and c-Myc. The study had a positive outcome with a development of iPSCs with antibody triggering the DNA sequencing response. It focused on the replacement of Oct4 using the same technique. However, it was not possible to find any replacement of fourth transcription gene factor Klf4.
The objective is now more concentrated on finding a fourth gene factor replacement to make the whole process shifted on antibody’s insertion for iPSCs production. And once we would be able to do it, we will have less number of negative outcomes.